Protect your family from respiratory illnesses. Schedule your immunization here >

Ranked nationally in pediatric care.
Arkansas Children's provides right-sized care for your child. U.S. News & World Report has ranked Arkansas Children's in seven specialties for 2025-2026.

It's easier than ever to sign up for MyChart.
Sign up online to quickly and easily manage your child's medical information and connect with us whenever you need.

We're focused on improving child health through exceptional patient care, groundbreaking research, continuing education, and outreach and prevention.

When it comes to your child, every emergency is a big deal.
Our ERs are staffed 24/7 with doctors, nurses and staff who know kids best – all trained to deliver right-sized care for your child in a safe environment.

Arkansas Children's provides right-sized care for your child. U.S. News & World Report has ranked Arkansas Children's in seven specialties for 2025-2026.

Looking for resources for your family?
Find health tips, patient stories, and news you can use to champion children.

Support from the comfort of your home.
Our flu resources and education information help parents and families provide effective care at home.

Children are at the center of everything we do.
We are dedicated to caring for children, allowing us to uniquely shape the landscape of pediatric care in Arkansas.

Transforming discovery to care.
Our researchers are driven by their limitless curiosity to discover new and better ways to make these children better today and healthier tomorrow.

We're focused on improving child health through exceptional patient care, groundbreaking research, continuing education, and outreach and prevention.

Then we're looking for you! Work at a place where you can change lives...including your own.

When you give to Arkansas Children's, you help deliver on our promise of a better today and a healthier tomorrow for the children of Arkansas and beyond

Become a volunteer at Arkansas Children's.
The gift of time is one of the most precious gifts you can give. You can make a difference in the life of a sick child.

Join our Grassroots Organization
Support and participate in this advocacy effort on behalf of Arkansas’ youth and our organization.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

When you give to Arkansas Children’s, you help deliver on our promise of a better today and a healthier tomorrow for the children of Arkansas and beyond.

Your volunteer efforts are very important to Arkansas Children's. Consider additional ways to help our patients and families.

Join one of our volunteer groups.
There are many ways to get involved to champion children statewide.

Make a positive impact on children through philanthropy.
The generosity of our supporters allows Arkansas Children's to deliver on our promise of making children better today and a healthier tomorrow.

Read and watch heart-warming, inspirational stories from the patients of Arkansas Children’s.

Hello.

Arkansas Children's Hospital
General Information 501-364-1100
Arkansas Children's Northwest
General Information 479-725-6800
Cleft Lip and Palate Program
The Cleft Lip and Palate Program at Arkansas Children's Hospital uses a comprehensive multidisciplinary team to provide your child's care. Each team member specializes in pediatric health. The team's goal is to ensure that care is provided in a coordinated, consistent manner. We schedule testing, appointments and treatments with your child's overall developmental, medical and psychological needs in mind.
The Cleft Lip and Palate Team at ACH is fully accredited by the American Cleft Palate Association (ACPA) and is one of many programs at ACH which provide high quality, individual service to children with special health care needs.
ENT surgeons, Dr. Larry Hartzell and Dr. Adam Johnson not only perform the primary cleft repair and bone grafting but provide comprehensive expertise in otologic and airway issues that may arise. Dr. Johnson also directs the Velopharyngeal Insufficiency Clinic (VPI) dedicated to both cleft and non-cleft patients experiencing speech disorders.
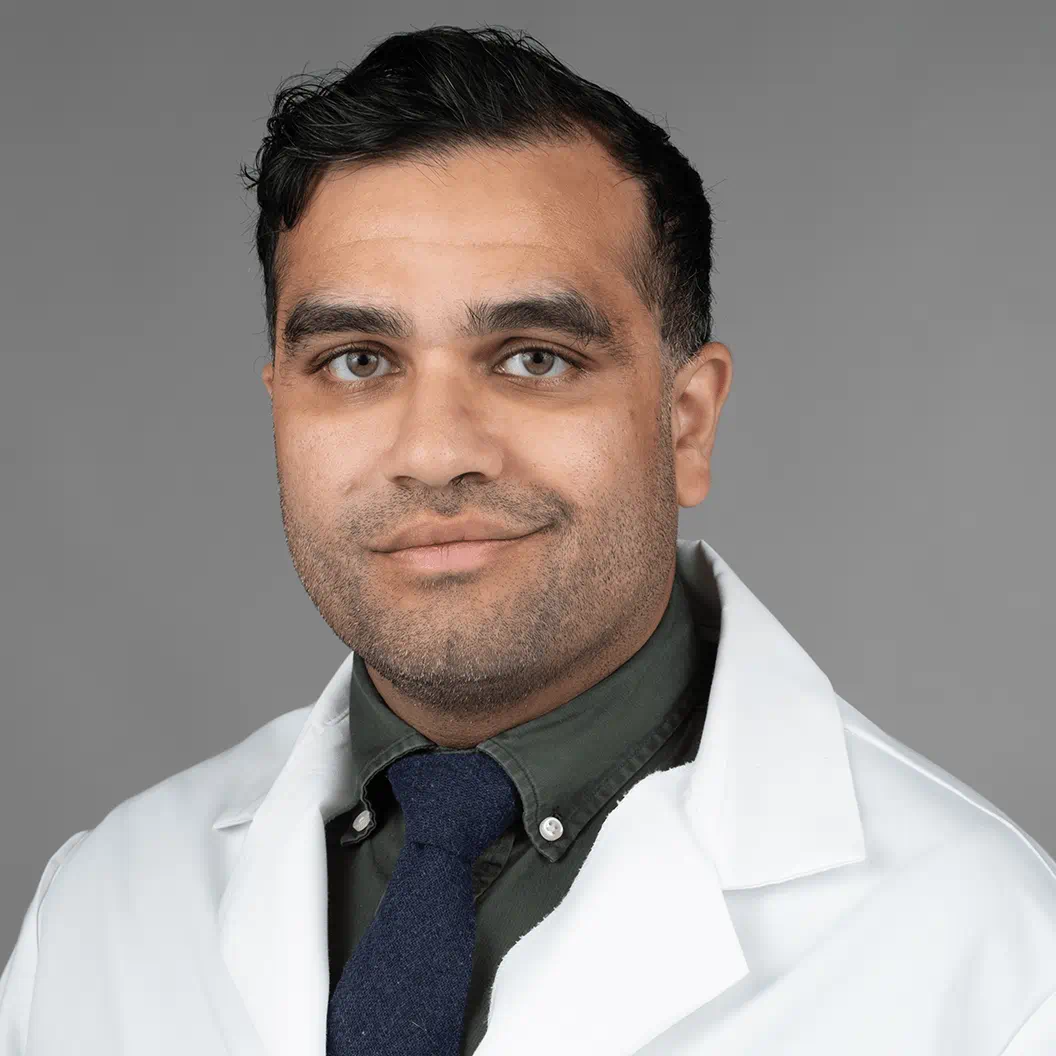
Plastic Surgeon, Dr. Sagar Mehta, chief of plastic and reconstructive surgery and craniofacial team director, specializes in primary cleft lip and palate surgery, alveolar bone grafting, orthognathic (jaw) surgeries, and cleft rhinoplasty.
Exceptional Cleft Lip and Palate Care for Children From Any Region

Possible Conditions
-
Cleft Lip and Cleft Palate
Learn more about cleft lip and cleft palate and how babies with these conditions are affected.
Treatments
Our Cleft Lip & Palate team has extensive experience treating all types of clefts and related disorders.
Nasoalveolar Molding (NAM)
NAM was originally developed by an ENT & Plastic Surgeon, Dr. Court Cutting, and craniofacial orthodontist, Dr. Barry Grayson at New York University (NYU) and is now available at Arkansas Children's. Not all babies with clefts are candidates for NAM, but for those that are, the retainer-like device can greatly help to narrow the width of the cleft, the gums and improve nasal shape.
Health at Home
Web Resources
We know the concern families must experience when a newborn is born with a cleft lip and palate condition. However, learning all you can about these conditions can help you understand your child’s situation and enable you to ask your doctor about any new developments in treatment. The following links provide the latest information on these important topics:
Camp Laughter Supports Patients
The cleft and craniofacial teams at Arkansas Children’s Hospital collaborate with Camp Aldersgate to provide a one-day camp for children living with cleft and craniofacial differences and their family members. Camp Laughter is a free annual event that occurs the first Saturday in August. This all-day event is for kids ages 5-18, who are in school and have a cleft or craniofacial difference. They can participate in various outdoor activities while connecting with other children just like them.
- For more information, contact camplaughter@archildrens.org.
- Give to Camp Laughter
Arkansas Children’s Cleft Team Provides Humanitarian Work in Ecuador
Adam Johnson, M.D., Ph.D., otolaryngologist, cleft surgeon and velopharyngeal insufficiency (VPI) clinic director, and Larry Hartzell, M.D., FAAP., director of cleft lip and palate program, have participated in several medical mission trips over the years and have made ongoing commitments to the organization. Read more about their missions. >
Important Facts
- Weight should be taken and recorded at least once every week
- Keep a feeding log with date, time, amount taken and length of feeding
- Feeding should last less than 25 minutes
- Most newborns during the first few weeks will feed 8-12 times per 24 hours
- Pumped breast milk and infant formula mixed with water should be the only liquids fed through bottles
Goals for your Baby
- Feeding for optimal, adequate growth and development
- Feeding should be less than 25 minutes
- Meet growth and weight goals for corrective surgery (8 pounds or more for lip repair and 18-20 pounds for palate repair)
- Limited pacifier use
- Baby foods fed by spoon starting at 4-6 months based on the feeding progression chart discussed with you by our clinic dietician
- At 6 months, or when there is good lip closure for spoon feeding, offer formula or breast milk from a cup
- Babies needing palate repair should be skilled at drinking from a cup before palate surgery
Types of Special Bottles
Pigeon Bottle –Y-cut nipple with one-way valve; contains an air valve to prevent collapsing while sucking. Large or small nipple options are available and assistive squeezing is possible.
Dr. Brown’s specialty bottle with one-way valve and air vent system to reduce gas.
Haberman bottle with one-way valve and variable flow rates; assistive squeezing is possible.
Tips for using specialty bottles
- Consult with Speech Pathology for bottle selection
- Do not screw the collar of bottle on too tight
- Hand clean bottle and nipples with warm soapy water and rinse well (do not boil or use in dishwasher)
- Replace nipples every 1-2 months
- Check with your surgeon’s clinic for a new supply
Feeding Your Baby
- Follow exact mixing and feeding instructions provided on discharge or in clinic
- Baby should be in a slightly reclined position during and after feeding
- Increase feeds weekly by 5 ml each feed. If you feed 60 ml feeds on discharge, then the next week feeds should be at 65 ml each and 70 ml the following week.
- Burp baby after every few ounces
- Clinic dietician will review infant feeding progression before introducing solid foods
- When child has progressed to table foods, avoid gummy or sticky foods or foods with sharp edges
Weight Gain Goals
Email or call your baby’s weight to the nutritionist weekly.
Goals for Weekly Weight Gain
| Age | Weight Goals |
| 1-3 months | 6-8 ounces |
| 4-6 months | 4-5 ounces |
| 7-12 months | 2-3 ounces |
Contact Info
For questions related to feeding your infant contact:
Karen Bright, MS, CLL-SLP
brightkl@archildrens.org
For questions related to your infant’s nutrition contact:
Joanna Daughety, RD, LD
Clinical Nutritionist, ENT Clinic
501-364-7541
daughetyj@archildrens.org
Helpful Websites:
Meet the Team
-

-

-
-

Peter Jang, DDS
Dentistry
Little Rock, Springdale -

-

Samantha Snavely, PA
Plastic and Reconstructive Surgery
Little Rock, Springdale -

Angie Zaki-Sabet, DMD
Dentistry
Little Rock
Audiologist - Since children with cleft palate have an increased risk of ear problems, ongoing audiological surveillance is necessary. The audiologist provides appropriate assessments for monitoring hearing status so that diagnosis and treatment can be made for any cleft-related hearing problems.
Dental Specialist - The dental specialists include the pediatric dentist, orthodontist, oral surgeon, periodontist, and prosthodontist. These specialists keep track of your child's dental growth and development and provide information on oral hygiene and dental treatment that may be necessary due to the cleft.
Geneticist - The geneticist alongside his genetic counselor, is available to discuss how clefts of the lip and palate occur and to answer questions about the risk of recurrence with future pregnancies. Later, this specialist can help your teenager understand the cause of a cleft and advise him or her about individual circumstances.
Neuropsychologist - The neuropsychologist is available to discuss you or your child's concerns.
Speech Pathologist - The speech pathologist will provide you with information about typical speech development along with suggestions for stimulation speech when your child is very young. Speech and swallowing dysfunction will be closely monitored and appropriate treatments or therapies will be prescribed at Arkansas Children's or if appropriate, closer to home.
Social Worker - The clinical social worker is available to meet with the family to assist in the psychosocial and emotional aspects of cleft lip/palate. This specialist is aware of services available in the community to which the family can be referred for information on medical coverage, financial assistance, and support groups/services.
Clinical Nutritionist - The nutritionist assists with any early feeding difficulties and monitors the child¹s nutritional intake. This specialist also provides follow-up of weight gain and height/weight parameters and provides information and support with specific diets related to some of the surgeries.
Registered Nurse - The nurse is available as a contact person to provide information and ensure that parents understand their child's health needs, treatment plan and follow-up. This specialist assists with the child's presurgical readiness and post-surgical recovery and provides instructions for home care.
Related Content
-
Patient Story
Arkansas Children’s ENT Expert Saves Teenage Bull Rider’s Life After Airway Explodes
Read the amazing story of Cayson Hall, who survived a near-fatal bull riding accident thanks to our ENT specialists.
-
Blog
What to Expect from Comprehensive Cleft Care at Arkansas Children’s
Learn about Arkansas Children's comprehensive cleft care and how it tailors support to your child's feeding, speech, and emotional well-being needs.
-
Patient Story
Shiloh Robertson: Shining Star for ENT, Endocrinology
Four-year-old Shiloh Robertson has overcome significant health challenges due to nasal pyriform aperture stenosis. Her family celebrates her resilience and the support from Arkansas Children's Hospital.
-
Blog
Ear Tubes: What They Are and Why Children Need Them
An Arkansas Children's otolaryngologist shares what parents need to know about ear tubes.
-
Patient Story
From NICU to Cleft: How Riley Has Triumphed at Arkansas Children’s Hospital
From NICU to Cleft. How Riley has triumphed at Arkansas Children’s Hospital.
-
Blog
Flat Skull? Ridge on the Head?
Discover how early detection of craniosynostosis can transform a child's life. Explore treatments from helmets to surgery at Arkansas Children's.
-
Blog
Does Your Child Snore? Here’s What to Know
Snoring is often considered an adult issue, but it can indicate an underlying condition in children. Arkansas Children's specializes in seeing patients that are newborn to 18 years of age for this issue.
Locations
Make an Appointment
Children may be referred for evaluation and treatment at the cleft clinic by physicians, speech therapists, teachers, families, guardians or others concerned with their general growth and development.
To make an appointment at the cleft clinic, please contact Jo McCallie, cleft team administrative assistant, at 501-364-7546, or Jordan Davis, cleft team coordinator, at 501-364-1658. Dr. Larry D. Hartzell, director of the cleft lip and palate program, can be reached via e-mail at cleftteam@archildrens.org.
- The Cleft Multidisciplinary Team Clinic meets the first Wednesday of each month.
- Regular, New and Follow-Up Cleft Clinics meet weekly and vary per surgeon.
-

-

Arkansas Children's Northwest
2601 Gene George Blvd.
Springdale, AR 72762
479-725-6800
View Location

Traveling to Arkansas Children's?
The Regional Care Center helps families traveling from another state or country receive world-class pediatric care before, during and after your stay.
Learn more about the Regional Care CenterRelated Services
-
Hospital Services
Arkansas Pediatric Aerodigestive Program
The Arkansas Children’s Aerodigestive Program constructed a multidisciplinary program that specializes in the diagnosis and surgical management of pediatric upper aerodigestive problems.
-
Hospital Services
Facial Plastic and Reconstructive Surgery
The Facial Plastic and Reconstructive Surgery Program at Arkansas Children's incorporates a multidisciplinary team to treat complex facial conditions.
-
Hospital Services
Ear, Nose and Throat Overview
Learn more about the comprehensive ENT care provided by our otolaryngology team.
-
Hospital Services
Thyroid Center
The Thyroid Center at Arkansas Children’s Hospital provides assessment for infants to young adults with thyroid nodules, thyroid cancer, hyperthyroidism, and hypothyroidism.
-
Hospital Services
Ear, Nose and Throat Treatments
Learn more about the treatment options provided by the ear, nose and throat experts at Arkansas Children's.
-
Hospital Services
Ear, Nose and Throat Resources for Health at Home
Our ENT news, resources and information help parents and families provide care at home.
-
Hospital Services
Craniofacial Orthodontics Clinic
Craniofacial Orthodontics. The craniofacial clinic offers comprehensive orthodontic services for patients with craniofacial and/or cleft lip/palate malformations.
-
Hospital Services
Ear Nose and Throat (Otolaryngology)
The otolaryngology team at Arkansas Children's provides comprehensive Ear, Nose and Throat care, including treatment for congenital anomalies and plastic and reconstructive surgery.
-
Hospital Services
Craniofacial and Pediatric Plastic Surgery
Our craniofacial, cleft and pediatric plastic surgery specialists at Arkansas Children’s are skilled in the surgical treatment of a range of congenital or acquired craniofacial conditions or issues for children of any age.
-
Hospital Services
Ear, Nose and Throat Conditions
Learn more about the broad range of ear, nose and throat (ENT) conditions treated by our pediatric otolaryngology team.

Arkansas Children's MyChart
Manage your child's medical information and connect with your Arkansas Children's medical team anytime online!
Log in to MyChart-
Hospital Services
Interpreter Services
Bookmark Interpreter ServicesArkansas Children's offers translation assistance to the hearing impaired as well as non-English speaking patients and families.
-
Hospital Services
Hospital Resources
Bookmark Hospital ResourcesAccess the information and tools you need to stay connected with Arkansas Children's quickly.
-
Hospital Services
Refer a Patient
Bookmark Refer a PatientArkansas Children's offers comprehensive care to patients through a physician referral.

